AHA/ACC/HFSA Guideline for the Management of Heart Failure (HF)
[American Heart Association/American College of Cardiology/Heart Failure Society of America 2022 Joint Committee Clinical Practice Guideline Update]
- A jointly published update to the clinical practice guideline for the management of heart failure (HF) was released in April 2022, with the intent of consolidating and replacing previous literature this includes the 2013 American College of Cardiology Foundation (ACCF)/AHA guideline for HF management and its subsequent 2017 focused update, which was developed by the ACC/AHA/HFSA.
- Up-to-date evidence incorporated into management recommendations emphasize the importance of applying clinical judgment and the role of shared decision-making with therapeutic approach.
What’s New from 2022?
Stages of HF, Redefined [1]
Emphasis on those who are at risk in staging → Focus on primary prevention in therapeutic management
| AHA/ACC/HFSA Staging | Definition | Goals of Therapy |
|---|---|---|
| A – At Risk for HF | – No previous or current symptoms/signs of HF – No structural/functional heart disease – No abnormal biomarkers – Patients with HTN, CVD, diabetes, obesity, exposure to cardiotoxic agents, genetic variant or family history for cardiomyopathy | – Primary prevention of heart failure |
| B – Pre-HF | – Patients with NO previous symptoms/signs of HF, but evidence of ONE of the following: A. Structural heart disease B. Evidence of increased filling pressures C. Risk factors PLUS Increased natriuretic peptide levels OR persistently elevated cardiac troponin | – Prevention of clinical heart failure |
| C – Symptomatic HF | – Previous or current symptoms/signs of HF AND – Structural heart disease | – Reduction of mortality – Reduction of symptoms and hospitalization risk – Elimination of potential barriers to self-care |
| D – Advanced HF | – Marked HF symptoms that interfere with daily life and/or recurrent HF hospitalizations despite attempts to optimize guideline-directed medical therapy (GDMT) | – Provision of inotropic support until mechanical support or cardiac transplantation available – Palliative symptom control and functional improvement (if not eligible for mechanical circulatory support or cardiac transplant) |
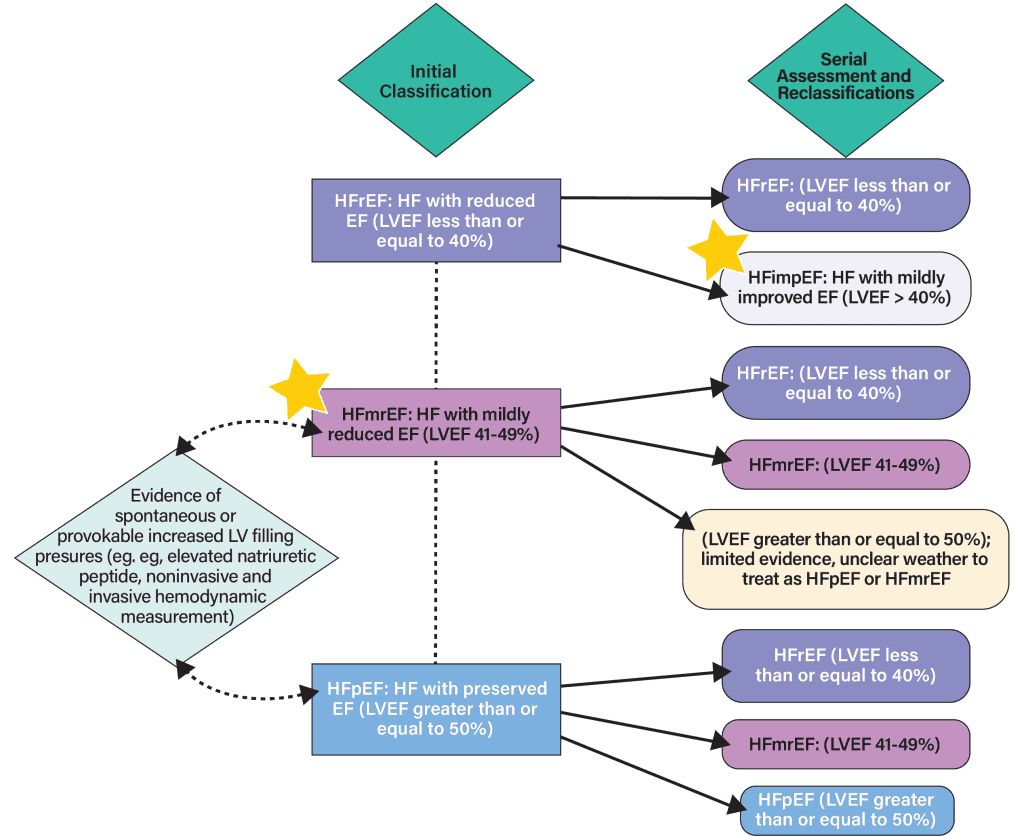
Classification of HF, Revised [1,2]
More appropriate classification of patient subgroups → Optimized guideline-directed medical therapy (GDMT)
Classification by New York Heart Association (NYHA)
- Classification of a patient’s disease is specified at baseline following initial diagnosis, and throughout the continuum of care; used by practitioners to determine eligibility for treatment strategies as it characterizes symptoms and functional capacity.
| NYHA Class I | No symptoms from ordinary daily activities |
| NYHA Class II | No symptoms at rest; ordinary daily physical activities cause HF symptoms |
| NYHA Class III | No symptoms at rest; activities lighter than ordinary daily physical activity causes HF symptoms |
| NYHA Class IV | Symptoms present at rest; discomfort worsens with physical activity |
- Patients with Stage C (symptomatic) HF can more appropriately be classified based on trajectory of symptoms, as tabulated below. Given the dynamic nature of HF, we must continuously assure the proper care is given – even with symptom resolution, the patient is still considered Stage C for management:
| Trajectory of Stage C Symptomatic HF | |
|---|---|
| New Onset/De Novo HF | – Newly diagnosed HF, no previous history |
| Resolution of Symptoms | – Resolution of symptoms/signs of HF… A. Previous HF symptoms resolved with persistent LV dysfunction → Stage C Patient B. Previous HF symptoms, signs, and structural abnormalities fully resolve → HF in Remission |
| Persistent HF | – Persistent HF with ongoing symptoms/signs and/or limited functional capacity |
| Worsening HF | – Worsening symptoms/signs/functional capacity |
Classification by Left Ventricular Ejection Fraction (LVEF) [1]
- LVEF classification is associated with differing patient prognoses and response to treatment; most clinical trials select patients based on ejection fraction.
Heart Failure Pharmacotherapy Recommendations + Expanded Role for SGLT2i [1,2]
| Guideline-Directed Medical Therapy (GDMT) Recommendations | ||
|---|---|---|
| Stage A | – Control blood pressure in patients with HTN – SGLT2i in patients with T2D PLUS: established CVD OR high CV risk – Manage existing comorbidities |
|
| Stage B | – ACEi and evidence-based BB in patients with LVEF ≤ 40% If LVEF ≤ 40% AND recent MI, use ARB if ACEi is not tolerated |
|
| Continue lifestyle modifications and management strategies implemented in Stage A, through Stage B | ||
| Stage C: HFpEF | – Diuretics as needed (loop preferred) – SGLT2i may be beneficial – May consider MRA, ARB/ARNi if LVEF is closer to 50% |
|
| Stage C: HFmrEF | – Diuretics as needed (loop preferred) – SGLT2i may be beneficial – May consider MRA, ACEi/ARB/ARNi, and evidence-based BB particularly if LVEF is closer to HFrEF threshold (LVEF ≤ 40%) |
|
| Stage C: HFimpEF | – Continue GDMT (even if asymptomatic) | |
| Stage C: HFrEF, persistent | All Patients | Special Populations |
| – ARNi or ACEi or ARB a. ARNi: NYHA class II-III b. ACEi or ARB: NYHA class II-IV c. Order of preference: ARNi > ACEi > ARB d. 36-hour washout required when switching between ACEi and ARNi (and vice versa) – Beta-blocker (evidence-based) a. Bisoprolol, carvedilol, metoprolol succinate – MRA (eg. eplerenone, spironolactone) a. NYHA class II-IV b. eGFR > 30mL/min/1.73m2 c. Serum potassium < 5 mEq/L – SGLT2i a. With or without T2D – Diuretics, as needed (loop preferred) |
– Hydralazine + isosorbide dinitrate
a. African American patients on optimal therapy b. NYHA class III-IV – Ivabradine a. NYHA class II-IV and LVEF ≤ 35% b. On GDMT, including max tolerated BB c. NSR with resting HR ≥ 70 BPM – Vericiguat a. NYHA class II-IV and LVEF < 45% b. Recent HR worsening c. Increased BNP or NT-proBNP – Digoxin a. If symptomatic despite GDMT OR b. Unable to tolerate GDMT – Potassium binders (eg. patiromer, sodium zirconium cyclosilicate) a. Patients with hyperkalemia (K+ ≥ 5.5mEq/L) while on RAASi – Omega-3 PUFA (may consider as adjunct) – NYHA class II-IV |
|
Abbreviations: HTN = hypertension, SGLT2i = sodium-glucose cotransporter-2 inhibitor, T2D = type II diabetes, CVD = cardiovascular disease, ACEi = angiotensin-converting enzyme inhibitor, BB = beta-blocker, MI = myocardial infarction, MRA = mineralocorticoid receptor antagonist, ARB = angiotensin II receptor blocker, ARNi = angiotensin receptor-neprilysin inhibitors, NSR = normal sinus rhythm, HR = heart rate, RAASi = renin-angiotensin-aldosterone system inhibitors, BPM = beats per minute.
See Appendix for details on medications by class and treatment guide for progression to Stage D; see guidelines for full information.
| Rationale of Recommendation for Use of SGLT2 Inhibitors in HF | ||
|---|---|---|
| Stage of HF | Rationale | Class of Recommendation |
| Stage A, At risk for HF | To prevent HF hospitalization in patients with T2D who have T2D who have CVD or are at high risk for CVD | 1 |
| Stage C, Symptomatic HF | ||
| HFrEF (LVEF ≤ 40%) | To reduce HF hospitalization and CV mortality in patients with symptomatic chronic HFrEF, regardless of the presence of T2D | 1 |
| HFpEF (LVEF ≥ 50%) | To reduce HF hospitalizations and CV mortality in patients | 2a |
| HRmrEF (LVEF 41-49%) | To reduce HF hospitalizations and CV mortality in patients | 2a |
Initial demonstration of improved rate of HF hospitalizations among patients with type 2 diabetes (T2D) at risk for HF → Further evidence accumulating on SGLT2 inhibitor CV benefit in patients with HF, regardless of presence of T2D (EMPULSE and DELIVER trials).
EMPULSE: Effects of Empagliflozin on Symptoms, Physical Limitations, and Quality of Life in Patients Hospitalized for Acute Heart Failure Who Have Been Stabilized.
DELIVER: Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction.
| Medications Commonly Used for HFrEF, Stage C HF (by drug class) | |||
|---|---|---|---|
| Initial Daily Dose(s) | Target Dose(s) | ||
| ACEi | captopril (Captoril) | 6.25 mg three times daily | 50 mg three times daily |
| enalapril (Vasotec) | 2.5 mg twice daily | 2.5 mg twice daily | |
| fosinopril (Monopril) | 5-10 mg once daily | 40 mg once daily | |
| lisinopril (Zestril) | 2.5-5 mg once daily | 20-40 mg once daily | |
| quinapril (Accupril) | 5 mg twice daily | 20 mg twice daily | |
| ramipril (Altace) | 1.25-2.5 mg once daily | 10 mg once daily | |
| ARB | candesartan (Atacand) | 4-8 mg once daily | 32 mg once daily |
| losartan (Cozaar) | 25-50 mg once daily | 50-150 mg once daily | |
| valsartan (Diovan) | 20-40 mg once daily | 160 mg twice daily | |
| ARNi | Sacubitril-valsartan (Entresto) | 49 mg sacubitril and 51 mg valsartan twice daily (therapy may be initiated at 24 mg sacubitril and 26 mg valsartan twice daily) | 97 mg sacubitril and 103 mg valsartan twice daily |
| SGLT2i | dapagliflozin (Farxiga) | 10 mg once daily | 10 mg once daily |
| empagliflozin (Jardiance) | 10 mg once daily | 10 mg once daily | |
| Beta Blockers | bisoprolol (Zebeta) | 1.25 mg once daily | 10 mg once daily |
| carvedilol (Coreg) | 3.125 mg twice daily | 25-50 mg twice daily | |
| carvedilol CR (Coreg CR) | 10 mg once daily | 80 mg once daily | |
| metoprolol succinate extended release (Toprol XL ) | 12.5-25 mg once daily | 200 mg once daily | |
| MRA | spironolactone (Aldactone) | 12.5-25 mg once daily | 25-50 mg once daily |
| eplerenone (Inspra) | 25 mg once daily | 50 mg once daily | |
| Loop diuretics (Oral) | bumetanide (Bumex) | 0.5-1.0 mg once or twice daily | MAX Daily Dose = 10 mg |
| furosemide (Lasix) | 20-40 mg once or twice daily | MAX Daily Dose = 600 mg | |
| torsemide (Demadex) | 10-20 mg once daily | MAX Daily Dose = 200 mg |
Resources:
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circ. 2022 Apr;145(18): e895-e1032.
- Implementing the 2022 ACC/AHA/ HFSA Guideline for the Management of Heart Failure: SGLT2 Inhibitors, Treatment Sequencing, and Value Statements. AJMC. 2022Jul29; 2022(Aug): 7-24.




