Diabetes Management Considerations for Older Adults
Diabetes is a highly prevalent health condition in the aging population. According to the American Diabetes Association (ADA), over 29% of people over the age of 65 years have diabetes. The number of older adults living with diabetes is expected to increase rapidly in the coming decades as the population ages and the effects of increasing obesity rates manifest in this population.
Diabetes management in older adults requires consideration and regular assessment of medical, psychological, functional, and social domains. When assessing older adults with diabetes, it is important to accurately categorize the type of diabetes, diabetes duration, the presence of complications and comorbidities, the individual’s capacity for self-management and availability of support systems, treatment burden, and treatment-related concerns, such as fear of hypoglycemia, polypharmacy, and financial barriers.
The 4Ms framework provides a helpful conceptual model to address person-specific issues that may affect diabetes management in older individuals and offers a framework to establish individualized treatment goals and approaches.
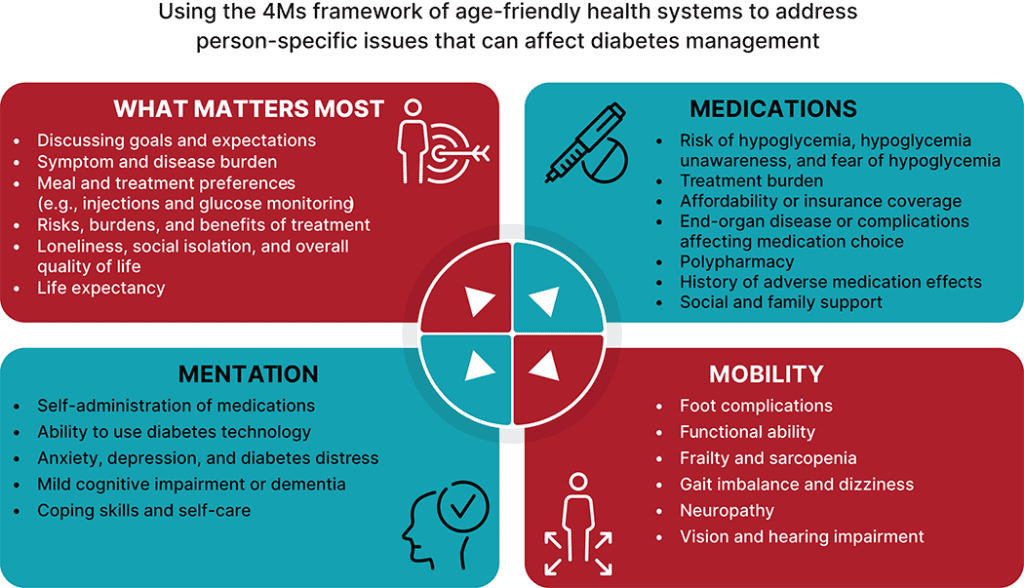
Figure 13.1 ADA Standards of Care in Diabetes: Older Adults – 2026
Determining Glycemic Goals for Older Adults
For 2026, the American Diabetes Association (ADA) emphasizes individualizing glycemic targets and increasing the use of technology to mitigate hypoglycemia risk in older adults. Providers should prioritize simplifying regimens and avoiding overtreatment for those with complex health needs to reduce symptomatic hyperglycemia and hypoglycemia.
This article will review the ADA’s latest recommendations and definitions concerning treatment goals and focus on managing hypoglycemia risk in community settings.
| Patient Characteristics/ Health Status | Rationale | Reasonable A1C goal‡ |
|---|---|---|
| Healthy (few coexisting chronic illnesses, intact cognitive and functional status). | Longer remaining life expectancy. | <7.0–7.5% (53–58 mmol/mol) |
| Complex/intermediate (multiple coexisting chronic illnesses* or two or more instrumental ADL impairments or mild-to-moderate cognitive impairment). | Variable remaining life expectancy, high treatment burden, hypoglycemia vulnerability, individual preference. | <8.0% (64 mmol/mol) |
| Very complex/poor health (LTC or end-stage chronic illnesses** or moderate-to-severe cognitive impairment or two or more ADL impairments). | Limited remaining life expectancy makes benefit minimal. | Avoid reliance on A1C; glucose control decisions should be based on avoiding hypoglycemia and symptomatic hyperglycemia. |
Table 13.2 Framework for considering treatment goals for glycemia in older adults with diabetes
The above table adapted from the ADA guidelines provides a decision-making framework for determining diabetes treatment goals in older adults, based on their health and functional status.
Simplification of glucose-lowering regimens can be achieved by either lowering the dose or discontinuing some medications, while monitoring glycemic response.
Re-evaluating glycemic goals through shared decision-making; de-intensifying, simplifying, or modifying treatments; and reassessing treatment burden has demonstrated to be safe and beneficial approaches in older adults. As patients’ disease burden progresses, the benefit of strict glycemic control diminishes.
The clinical pharmacist involved in care is an excellent resource to consult in the simplification of diabetes regimens and utilization of safer therapeutic options.
Hypoglycemia Risk Assessment
Older adults in community care and PALTC settings are especially vulnerable to hypoglycemia. They have a disproportionately high number of health conditions that can increase hypoglycemia risk: impaired cognitive and renal function, slowed hormonal regulation and counter-regulation, suboptimal hydration, variable appetite and nutritional intake, requirement for feeding assistance, polypharmacy, and slowed intestinal absorption.
Intensive glycemic management in older adults, particularly those with complex health status, with medication plans that increase the risk of hypoglycemia through use of insulin and/or sulfonylureas, is considered overtreatment and may increase the risk of mortality.
| Clinical and Biological Risk Factors | |
|---|---|
Other risk factors
|
|
Table 6.5 Assessment of hypoglycemia risk
Rates of hypoglycemia are highest for individuals treated with intensive insulin therapy (including multiple daily injections of insulin, continuous subcutaneous insulin infusion, or automated insulin delivery systems), followed by basal insulin, then sulfonylureas or meglitinides. Combining treatment with insulin and sulfonylureas further increases hypoglycemia risk.
Hypoglycemia Classification & Monitoring
In older adults, hypoglycemia symptoms are often “masked” or difficult to recognize due to age-related physiological changes, cognitive impairment, and medication effects. The ADA’s classification for hypoglycemic events with common symptoms provided below:
| Glycemic Criteria/Description | |
|---|---|
| Level 1 | Glucose <70 mg/dL (<3.9 mmol/L) and ≥54 mg/dL (≥3.0 mmol/L)
|
| Level 2 | Glucose <54 mg/dL (<3.0 mmol/L)
|
| Level 3 | A severe event characterized by altered mental and/or physical status requiring assistance for treatment of hypoglycemia, irrespective of glucose level |
Table 6.4 Classification of hypoglycemia
Hypoglycemia has a broad range of negative health consequences. Level 3 hypoglycemia may be recognized or unrecognized and can progress to loss of consciousness, seizure, coma, or death.
Level 2 or 3 hypoglycemic events should trigger a re-evaluation of the individual’s diabetes treatment plan, with consideration of deintensification of therapy within individualized glycemic goals.
The ADA in recent years has added several recommendations for leveraging diabetes care technology, specifically continuous glucose monitors (CGM) and insulin delivery devices to improve glycemic control and reduce hypoglycemia events, even in older adults.
CGMs are currently recommended for older adults with type 1 diabetes and type 2 diabetes on insulin therapy to improve glycemic outcomes, reduce hypoglycemia, and reduce treatment burden.
*adapted with permission from the American Society of Consultant Pharmacists (ASCP)
References:
- Older Adults (Section 13): American Diabetes Association Professional Practice Committee. 13. Older Adults: Standards of Care in Diabetes—2026. Diabetes Care 2026;49(Supplement_1):S259–S279. DOI: 10.2337/dc26-S013.
- Glycemic Goals (Section 6): American Diabetes Association Professional Practice Committee. 6. Glycemic Goals, Hypoglycemia, and Hyperglycemic Crises: Standards of Care in Diabetes—2026. Diabetes Care 2026;49(Supplement_1):S124–S149. DOI: 10.2337/dc26-S006




