What are Anticholinergic Drugs?
Anticholinergic medications (‘anticholinergics’) are drugs that block and inhibit the activity of the neurotransmitter acetylcholine found in the central and peripheral nervous system. In doing so, these drugs inhibit the actions of the parasympathetic nervous system (‘rest and digest’) via selective blockade of acetylcholine from binding to its neuronal receptors. Acetylcholine is responsible for regulating and transmitting signals involved in the actions of smooth muscle located in the GI tract, lungs, urinary tract, and other areas of the body.
Anticholinergic drugs are used to treat a variety of conditions, including chronic obstructive pulmonary disease (COPD), bladder conditions, allergies, gastrointestinal disorders, and symptoms of Parkinson’s disease. This article discusses the risks associated with anticholinergic drug use in older adults and tools to help guide therapy selection to reduce anticholinergic burden in this population.
Anticholinergic Drugs Pose Significant Risk to the Older Adult
Anticholinergic drugs can cause a range of side effects, including dry mouth, constipation, urinary retention, blurred vision, and increased heart rate. These side effects can be particularly problematic in the elderly, who may already be prone to dehydration, constipation, and urinary issues.
Elderly individuals are already at a higher risk of falls due to age-related changes in balance, muscle strength, and coordination. Anticholinergic medications can further increase this risk by causing dizziness, blurred vision, and impaired motor function.
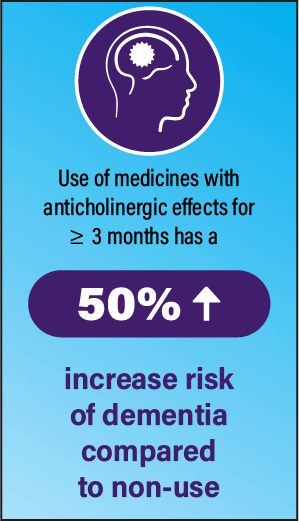
Anticholinergic medications can also have negative effects on cognition, particularly in elderly patients who may already be at risk for cognitive decline or have underlying cognitive impairments such as dementia. These drugs can cause confusion, memory problems, and impair attention and executive functions.
Medications with Strong Anticholinergic Properties
Anticholinergic drugs have their place in therapy, however considering the risks to older adults, geriatric minded practitioners may want to avoid use of strong anticholinergic drugs, and consider the total anticholinergic effect of concurrent medications, known as ‘cumulative anticholinergic burden’.
The 2023 AGS Beers Criteria helps define which medications are considered strongly anticholinergic, and therefore potentially inappropriate for older adults. The table below summarizes by drug category.
2023 AGS Beers Criteria – Drugs With Strong Anticholinergic Properties
| Antidepressants | Antiemetics | Antihistamines (first-generation) | Antimuscarinics (incontinence) |
| ■ Amitriptyline ■ Amoxapine ■ Clomipramine ■ Desipramine ■ Doxepin (> 6 mg daily) ■ Imipramine ■ Nortriptyline ■ Paroxetine | ■ Prochlorperazine ■ Promethazine | ■ Brompheniramine ■ Chlorpheniramine ■ Cyproheptadine ■ Dimenhydrinate ■ Diphenhydramine ■ Doxylamine ■ Hydroxyzine ■ Meclizine ■ Promethazine ■ Triprolidine ■ Promethazine ■ Triprolidine | ■ Darifenacin ■ Fesoterodine ■ Flavoxate ■ Oxybutynin ■ Solifenacin ■ Tolterodine ■ Trospium |
| Antiparkinsonian agents | Antipsychotics | Antispasmodics | Skeletal muscle relaxants |
| ■ Benztropine ■ Trihexyphenidyl | ■ Chlorpromazine ■ Clozapine ■ Olanzapine ■ Perphenazine | ■ Atropine ■ Clidiuniumchlordiazepoxide ■ Dicyclomine ■ Homatropine ■ Hyoscyamine ■ Scopolamine | ■ Cyclobenzaprine ■ Orphenadrine |

Cumulative Anticholinergic Burden (ACB)
Total anticholinergic effect, or cumulative anticholinergic burden, increases when drugs with strong anticholinergic properties or combinations of anticholinergic drugs are prescribed.
Older patients are more likely to have multiple co-morbidities and as a result, polypharmacy that includes anticholinergic medications. As the body ages, its ability to metabolize medications declines, the permeability of their blood-brain barrier increases, and therefore older patients are more susceptible to the anticholinergic effects of their medications.
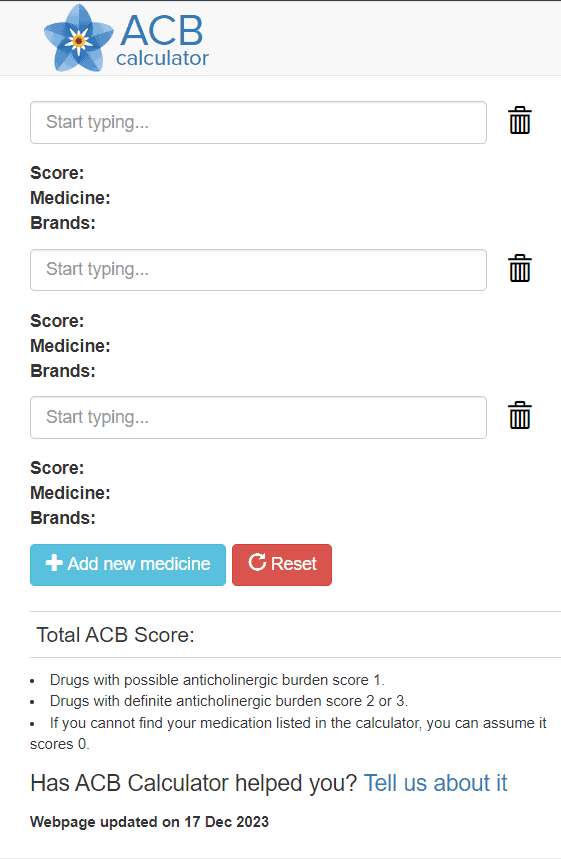
Various anticholinergic scales have been developed in clinical studies to quantify the effects of these medications and provide a practical tool for optimizing drug selection in older patients. Most offer a 1-3 scale for describing anticholinergic activity of medications; 1- minimal, 2-mild or moderate, 3-strong or severe. Higher cumulative scores are associated with increased anticholinergic burden and risk for related adverse effects.
Of the resources available online, the scorecard and calculator at www.acbcalc.com is free to access and easy to use. They integrate two of the more reliable anticholinergic scales into their scorecard and cite a cumulative burden of 3+ to be associated with an increased risk for cognitive impairment.
Reducing Anticholinergic Medication Burden
Taking action to reduce anticholinergic burden for our older adult population is an important intervention to promote the individual’s longevity and reduce the potential for significant adverse effects. Evaluate strong anticholinergic medications for deprescribing opportunities, dose reduction or choose alternative therapy with less anticholinergic activity. Every anticholinergic drug has a cumulative effect, and so any reduction to overall anticholinergic burden will have a positive impact.
If your patient presents with symptoms that may be related to anticholinergic medication (dry eyes, urinary retention, constipation, etc.), engage the provider and pharmacist in care of that patient for a comprehensive medication review to identify contributing anticholinergic medications, as symptoms will often alleviate with a reduction in anticholinergic burden.
References:
- American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71(7):2052-2081. doi:10.1111/jgs.18372
- ACB Calculator. Available from: https://www.acbcalc.com/
- Lozano-Ortega, Johnston, Cheung, et al. A review of published anticholinergic scales and measures and their applicability in database analyses. Archives of Gerontology and Geriatrics. 2020. https://doi.org/10.1016/j.archger.2019.05.010
- Dmochowski, Thai, Iglay, et al. Increased risk of incident dementia following use of anticholinergic agents: A systematic literature review and meta-analysis. Neurourol Urodyn. 2021 Jan;40(1):28-37. doi: 10.1002/nau.24536. Epub 2020 Oct 23. PMID: 33098213; PMCID: PMC7821204.




